Molecular characterization of chordoma xenografts generated from a novel primary chordoma cell source and two chordoma cell lines.
Karikari, IO; Gilchrist, CL; Jing, L; Alcorta, DA; Chen, J; Richardson, WJ; Gabr, MA; Bell, RD; Kelley, MJ; Bagley, CA; Setton, LA
Journal of neurosurgery. Spine
21
386-93
2014
Show Abstract
Chordoma cells can generate solid-like tumors in xenograft models that express some molecular characteristics of the parent tumor, including positivity for brachyury and cytokeratins. However, there is a dearth of molecular markers that relate to chordoma tumor growth, as well as the cell lines needed to advance treatment. The objective in this study was to isolate a novel primary chordoma cell source and analyze the characteristics of tumor growth in a mouse xenograft model for comparison with the established U-CH1 and U-CH2b cell lines.Primary cells from a sacral chordoma, called "DVC-4," were cultured alongside U-CH1 and U-CH2b cells for more than 20 passages and characterized for expression of CD24 and brachyury. While brachyury is believed essential for driving tumor formation, CD24 is associated with healthy nucleus pulposus cells. Each cell type was subcutaneously implanted in NOD/SCID/IL2Rγ(null) mice. The percentage of solid tumors formed, time to maximum tumor size, and immunostaining scores for CD24 and brachyury (intensity scores of 0-3, heterogeneity scores of 0-1) were reported and evaluated to test differences across groups.The DVC-4 cells retained chordoma-like morphology in culture and exhibited CD24 and brachyury expression profiles in vitro that were similar to those for U-CH1 and U-CH2b. Both U-CH1 and DVC-4 cells grew tumors at rates that were faster than those for U-CH2b cells. Gross tumor developed at nearly every site (95%) injected with U-CH1 and at most sites (75%) injected with DVC-4. In contrast, U-CH2b cells produced grossly visible tumors in less than 50% of injected sites. Brachyury staining was similar among tumors derived from all 3 cell types and was intensely positive (scores of 2-3) in a majority of tissue sections. In contrast, differences in the pattern and intensity of staining for CD24 were noted among the 3 types of cell-derived tumors (p less than 0.05, chi-square test), with evidence of intense and uniform staining in a majority of U-CH1 tumor sections (score of 3) and more than half of the DVC-4 tumor sections (scores of 2-3). In contrast, a majority of sections from U-CH2b cells stained modestly for CD24 (scores of 1-2) with a predominantly heterogeneous staining pattern.This is the first report on xenografts generated from U-CH2b cells in which a low tumorigenicity was discovered despite evidence of chordoma-like characteristics in vitro. For tumors derived from a primary chordoma cell and U-CH1 cell line, similarly intense staining for CD24 was observed, which may correspond to their similar potential to grow tumors. In contrast, U-CH2b tumors stained less intensely for CD24. These results emphasize that many markers, including CD24, may be useful in distinguishing among chordoma cell types and their tumorigenicity in vivo. | 24905390
 |
Homeodomain interacting protein kinase 2 regulates postnatal development of enteric dopaminergic neurons and glia via BMP signaling.
Chalazonitis, A; Tang, AA; Shang, Y; Pham, TD; Hsieh, I; Setlik, W; Gershon, MD; Huang, EJ
The Journal of neuroscience : the official journal of the Society for Neuroscience
31
13746-57
2011
Show Abstract
Trophic factor signaling is important for the migration, differentiation, and survival of enteric neurons during development. The mechanisms that regulate the maturation of enteric neurons in postnatal life, however, are poorly understood. Here, we show that transcriptional cofactor HIPK2 (homeodomain interacting protein kinase 2) is required for the maturation of enteric neurons and for regulating gliogenesis during postnatal development. Mice lacking HIPK2 display a spectrum of gastrointestinal (GI) phenotypes, including distention of colon and slowed GI transit time. Although loss of HIPK2 does not affect the enteric neurons in prenatal development, a progressive loss of enteric neurons occurs during postnatal life in Hipk2(-/-) mutant mice that preferentially affects the dopaminergic population of neurons in the caudal region of the intestine. The mechanism by which HIPK2 regulates postnatal enteric neuron development appears to involve the response of enteric neurons to bone morphogenetic proteins (BMPs). Specifically, compared to wild type mice, a larger proportion of enteric neurons in Hipk2(-/-) mutants have an abnormally high level of phosphorylated Smad1/5/8. Consistent with the ability of BMP signaling to promote gliogenesis, Hipk2(-/-) mutants show a significant increase in glia in the enteric nervous system. In addition, numbers of autophagosomes are increased in enteric neurons in Hipk2(-/-) mutants, and synaptic maturation is arrested. These results reveal a new role for HIPK2 as an important transcriptional cofactor that regulates the BMP signaling pathway in the maintenance of enteric neurons and glia, and further suggest that HIPK2 and its associated signaling mechanisms may be therapeutically altered to promote postnatal neuronal maturation. | 21957238
 |
Targeted cell replacement with bone marrow cells for airway epithelial regeneration.
Wong, AP; Dutly, AE; Sacher, A; Lee, H; Hwang, DM; Liu, M; Keshavjee, S; Hu, J; Waddell, TK
American journal of physiology. Lung cellular and molecular physiology
293
L740-52
2007
Show Abstract
It has been suggested that some adult bone marrow cells (BMC) can localize to the lung and develop tissue-specific characteristics including those of pulmonary epithelial cells. Here, we show that the combination of mild airway injury (naphthalene-induced) as a conditioning regimen to direct the site of BMC localization and transtracheal delivery of short-term cultured BMC enhances airway localization and adoption of an epithelial-like phenotype. Confocal analysis of airway and alveolar-localized BMC (fluorescently labeled) with epithelial markers shows expression of the pulmonary epithelial proteins, Clara cell secretory protein, and surfactant protein C. To confirm epithelial gene expression by BMC, we generated transgenic mice expressing green fluorescent protein (GFP) driven by the epithelial-specific cytokeratin-18 promoter and injected BMC from these mice transtracheally into wild-type recipients after naphthalene-induced airway injury. BMC retention in the lung was observed for at least 120 days following cell delivery with increasing GFP transgene expression over time. Some BMC cultured in vitro over time also expressed GFP transgene, suggesting epithelial transdifferentiation of the BMC. The results indicate that targeted delivery of BMC can promote airway regeneration. | 17616650
 |
Identification of pulmonary Oct-4+ stem/progenitor cells and demonstration of their susceptibility to SARS coronavirus (SARS-CoV) infection in vitro.
Ling, TY; Kuo, MD; Li, CL; Yu, AL; Huang, YH; Wu, TJ; Lin, YC; Chen, SH; Yu, J
Proceedings of the National Academy of Sciences of the United States of America
103
9530-5
2006
Show Abstract
In this study, we report a serum-free culture system for primary neonatal pulmonary cells that can support the growth of octamer-binding transcription factor 4+ (Oct-4+) epithelial colonies with a surrounding mesenchymal stroma. In addition to Oct-4, these cells also express other stem cell markers such as stage-specific embryonic antigen 1 (SSEA-1), stem cell antigen 1 (Sca-1), and Clara cell secretion protein (CCSP) but not c-Kit, CD34, and p63, indicating that they represent a subpopulation of Clara cells that have been implicated as lung stem/progenitor cells in lung injury models. These colony cells can be kept for weeks in primary cultures and undergo terminal differentiation to alveolar type-2- and type-1-like pneumocytes sequentially when removed from the stroma. In addition, we have demonstrated the presence of Oct-4+ long-term BrdU label-retaining cells at the bronchoalveolar junction of neonatal lung, providing a link between the Oct-4+ cells in vivo and in vitro and strengthening their identity as putative neonatal lung stem/progenitor cells. Lastly, these Oct-4+ epithelial colony cells, which also express angiotensin-converting enzyme 2, are the target cells for severe acute respiratory syndrome coronavirus infection in primary cultures and support active virus replication leading to their own destruction. These observations imply the possible involvement of lung stem/progenitor cells, in addition to pneumocytes, in severe acute respiratory syndrome coronavirus infection, accounting for the continued deterioration of lung tissues and apparent loss of capacity for lung repair. | 16772384
 |
Gene and stem cell therapy of the hair follicle.
Robert M Hoffman
Methods in molecular biology (Clifton, N.J.)
289
437-48
2005
Show Abstract
The hair follicle is a highly complex appendage of the skin containing a multiplicity of cell types. The follicle undergoes constant cycling through the life of the organism including growth and resorption with growth dependent on specific stem cells. The targeting of the follicle by genes and stem cells to change its properties, in particular, the nature of the hair shaft is discussed. Hair follicle delivery systems are described such as liposomes and viral vectors for gene therapy. The nature of the hair follicle stem cells is discussed, in particular, its pluripotency. | 15502205
 |
Nestin expression in hair follicle sheath progenitor cells.
Li, L; Mignone, J; Yang, M; Matic, M; Penman, S; Enikolopov, G; Hoffman, RM
Proceedings of the National Academy of Sciences of the United States of America
100
9958-61
2003
Show Abstract
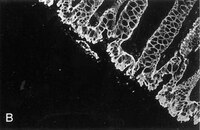
The intermediate filament protein, nestin, marks progenitor cells of the CNS. Such CNS stem cells are selectively labeled by placing GFP under the control of the nestin regulatory sequences. During early anagen or growth phase of the hair follicle, nestin-expressing cells, marked by GFP fluorescence in nestin-GFP transgenic mice, appear in the permanent upper hair follicle immediately below the sebaceous glands in the follicle bulge. This is where stem cells for the hair follicle outer-root sheath are thought to be located. The relatively small, oval-shaped, nestin-expressing cells in the bulge area surround the hair shaft and are interconnected by short dendrites. The precise locations of the nestin-expressing cells in the hair follicle vary with the hair cycle. During telogen or resting phase and in early anagen, the GFP-positive cells are mainly in the bulge area. However, in mid- and late anagen, the GFP-expressing cells are located in the upper outer-root sheath as well as in the bulge area but not in the hair matrix bulb. These observations show that the nestin-expressing cells form the outer-root sheath. Results of the immunohistochemical staining showed that nestin, GFP, keratin 5/8, and keratin 15 colocalize in the hair follicle bulge cells, outer-root sheath cells, and basal cells of the sebaceous glands. These data indicate that nestin-expressing cells, marked by GFP, in the hair follicle bulge are indeed progenitors of the follicle outer-root sheath. The expression of the unique protein, nestin, in both neural stem cells and hair follicle stem cells suggests their possible relation. Full Text Article | 12904579
 |
Keratin expression in cervical cancer.
Smedts, F, et al.
Am. J. Pathol., 141: 497-511 (1992)
1992
Show Abstract
Using a panel of 21 monoclonal and 2 polyclonal keratin antibodies, capable of detecting separately 11 subtypes of their epithelial intermediate filament proteins at the single cell level, we investigated keratin expression in 16 squamous cell carcinomas, 9 adenocarcinomas, and 3 adenosquamous carcinomas of the human uterine cervix. The keratin phenotype of the keratinizing squamous cell carcinoma was found to be most complex comprising keratins 4, 5, 6, 8, 13, 14, 16, 17, 18, 19, and usually keratin 10. The nonkeratinizing variety of the squamous cell carcinoma expressed keratins 6, 14, 17, and 19 in all cases, usually 4, 5, 7, 8, and 18, and sometimes keratins 10, 13, and 16. Adenocarcinomas displayed a less complex keratin expression pattern comprising keratins 7, 8, 17, 18, and 19, while keratin 14 was often present and keratins 4, 5, 10 and 13 were sporadically found in individual cells in a few cases. These keratin phenotypes may be useful in differential diagnostic considerations when distinguishing between keratinizing and nonkeratinizing carcinomas (using keratin 10, 13, and 16 antibodies), and also in the distinction between nonkeratinizing carcinomas and poorly differentiated adenocarcinomas, which do not express keratins 5 and 6. Keratin 17 may also be useful in distinguishing carcinomas of the cervix from those of the colon and also from mesotheliomas. Furthermore the presence of keratin 17 in a CIN I, II, or III lesion may indicate progressive potential while its absence could be indicative of a regressive behavior. Because most carcinomas express keratins 8, 14, 17, 18, and 19, we propose that this expression pattern reflects the origin of cervical cancer from a common progenitor cell, i.e., the endocervical reserve cell that has been shown to express keratins 5, 8, 14, 17, 18, and 19. | 1379783
 |
Assembly of amino-terminally deleted desmin in vimentin-free cells.
Raats, J M, et al.
J. Cell Biol., 111: 1971-85 (1990)
1990
Show Abstract
To study the role of the amino-terminal domain of the desmin subunit in intermediate filament (IF) formation, several deletions in the sequence encoding this domain were made. The deleted hamster desmin genes were fused to the RSV promoter. Expression of such constructs in vimentin-free MCF-7 cells as well as in vimentin-containing HeLa cells, resulted in the synthesis of mutant proteins of the expected size. Single- and double-label immunofluorescence assays of transfected cells showed that in the absence of vimentin, desmin subunits missing amino acids 4-13 are still capable of filament formation, although in addition to filaments large numbers of desmin dots are present. Mutant desmin subunits missing larger portions of their amino terminus cannot form filaments on their own. It may be concluded that the amino-terminal region comprising amino acids 7-17 contains residues indispensable for desmin filament formation in vivo. Furthermore it was shown that the endogenous vimentin IF network in HeLa cells masks the effects of mutant desmin on IF assembly. Intact and mutant desmin colocalized completely with endogenous vimentin in HeLa cells. Surprisingly, in these cells endogenous keratin also seemed to colocalize with endogenous vimentin, even if the endogenous vimentin filaments were disturbed after expression of some of the mutant desmin proteins. In MCF-7 cells some overlap between endogenous keratin and intact exogenous desmin filaments was also observed, but mutant desmin proteins did not affect the keratin IF structures. In the absence of vimentin networks (MCF-7 cells), the initiation of desmin filament formation seems to start on the preexisting keratin filaments. However, in the presence of vimentin (HeLa cells) a gradual integration of desmin in the preexisting vimentin filaments apparently takes place. | 1699950
 |
Tissue distribution of keratin 7 as monitored by a monoclonal antibody.
Ramaekers, F, et al.
Exp. Cell Res., 170: 235-49 (1987)
1987
Show Abstract
Monoclonal antibody (RCK 105) directed against keratin 7 was obtained after immunization of BALB/c mice with cytoskeletal preparations from T24 cells and characterized by one- (1D) and two-dimensional (2D) immunoblotting. In cultured epithelial cells, known from gel electrophoretic studies to contain keratin 7, this antibody gives a typical keratin intermediate filament staining pattern, comparable to that obtained with polyclonal rabbit antisera to skin keratins or with other monoclonal antibodies, recognizing for example keratins 5 and 8 or keratin 18. Using RCK 105, the distribution of keratin 7 throughout human epithelial tissues was examined and correlated with expression patterns of other keratins. Keratin 7 was found to occur in the columnar and glandular epithelium of the lung, cervix, breast, in bile ducts, collecting ducts in the kidney and in mesothelium, but to be absent from gastrointestinal epithelium, hepatocytes, proximal and distal tubules of the kidney and myoepithelium. Nor could it be detected in the stratified epithelia of the skin, tongue, esophagus, or cervix but strongly stained all cell layers of the urinary bladder transitional epithelium. When applied to carcinomas derived from these different tissue types it became obvious that an antibody to keratin 7 may allow an immunohistochemical distinction between certain types of adenocarcinomas. | 2436934
 |