Exposure of neonatal rats to alcohol has differential effects on neuroinflammation and neuronal survival in the cerebellum and hippocampus.
Topper, LA; Baculis, BC; Valenzuela, CF
Journal of neuroinflammation
12
160
2015
Show Abstract
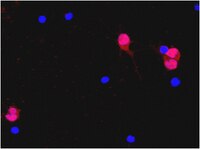
Fetal alcohol exposure is a leading cause of preventable birth defects, yet drinking during pregnancy remains prevalent worldwide. Studies suggest that activation of the neuroimmune system plays a role in the effects of alcohol exposure during the rodent equivalent to the third trimester of human pregnancy (i.e., first week of neonatal life), particularly by contributing to neuronal loss. Here, we performed a comprehensive study investigating differences in the neuroimmune response in the cerebellum and hippocampus, which are important targets of third trimester-equivalent alcohol exposure.To model heavy, binge-like alcohol exposure during this period, we exposed rats to alcohol vapor inhalation during postnatal days (P)3-5 (blood alcohol concentration = 0.5 g/dL). The cerebellar vermis and hippocampus of rat pups were analyzed for signs of glial cell activation and neuronal loss by immunohistochemistry at different developmental stages. Cytokine production was measured by reverse transcriptase polymerase chain reaction during peak blood alcohol concentration and withdrawal periods. Additionally, adolescent offspring were assessed for alterations in gait and spatial memory.We found that this paradigm causes Purkinje cell degeneration in the cerebellar vermis at P6 and P45; however, no signs of neuronal loss were found in the hippocampus. Significant increases in pro-inflammatory cytokines were observed in both brain regions during alcohol withdrawal periods. Although astrocyte activation occurred in both the hippocampus and cerebellar vermis, microglial activation was observed primarily in the latter.These findings suggest that heavy, binge-like third trimester-equivalent alcohol exposure has time- and brain region-dependent effects on cytokine levels, morphological activation of microglia and astrocytes, and neuronal survival. | 26337952
 |
Differential sensitivity of prefrontal cortex and hippocampus to alcohol-induced toxicity.
Fowler, AK; Thompson, J; Chen, L; Dagda, M; Dertien, J; Dossou, KS; Moaddel, R; Bergeson, SE; Kruman, II
PloS one
9
e106945
2014
Show Abstract
The prefrontal cortex (PFC) is a brain region responsible for executive functions including working memory, impulse control and decision making. The loss of these functions may ultimately lead to addiction. Using histological analysis combined with stereological technique, we demonstrated that the PFC is more vulnerable to chronic alcohol-induced oxidative stress and neuronal cell death than the hippocampus. This increased vulnerability is evidenced by elevated oxidative stress-induced DNA damage and enhanced expression of apoptotic markers in PFC neurons. We also found that one-carbon metabolism (OCM) impairment plays a significant role in alcohol toxicity to the PFC seen from the difference in the effects of acute and chronic alcohol exposure on DNA repair and from exaggeration of the damaging effects upon additional OCM impairment in mice deficient in a key OCM enzyme, methylenetetrahydrofolate reductase (MTHFR). Given that damage to the PFC leads to loss of executive function and addiction, our study may shed light on the mechanism of alcohol addiction. | 25188266
 |
Alcohol-induced one-carbon metabolism impairment promotes dysfunction of DNA base excision repair in adult brain.
Fowler, AK; Hewetson, A; Agrawal, RG; Dagda, M; Dagda, R; Moaddel, R; Balbo, S; Sanghvi, M; Chen, Y; Hogue, RJ; Bergeson, SE; Henderson, GI; Kruman, II
The Journal of biological chemistry
287
43533-42
2012
Show Abstract
The brain is one of the major targets of chronic alcohol abuse. Yet the fundamental mechanisms underlying alcohol-mediated brain damage remain unclear. The products of alcohol metabolism cause DNA damage, which in conditions of DNA repair dysfunction leads to genomic instability and neural death. We propose that one-carbon metabolism (OCM) impairment associated with long term chronic ethanol intake is a key factor in ethanol-induced neurotoxicity, because OCM provides cells with DNA precursors for DNA repair and methyl groups for DNA methylation, both critical for genomic stability. Using histological (immunohistochemistry and stereological counting) and biochemical assays, we show that 3-week chronic exposure of adult mice to 5% ethanol (Lieber-Decarli diet) results in increased DNA damage, reduced DNA repair, and neuronal death in the brain. These were concomitant with compromised OCM, as evidenced by elevated homocysteine, a marker of OCM dysfunction. We conclude that OCM dysfunction plays a causal role in alcohol-induced genomic instability in the brain because OCM status determines the alcohol effect on DNA damage/repair and genomic stability. Short ethanol exposure, which did not disturb OCM, also did not affect the response to DNA damage, whereas additional OCM disturbance induced by deficiency in a key OCM enzyme, methylenetetrahydrofolate reductase (MTHFR) in Mthfr(+/-) mice, exaggerated the ethanol effect on DNA repair. Thus, the impact of long term ethanol exposure on DNA repair and genomic stability in the brain results from OCM dysfunction, and MTHFR mutations such as Mthfr 677C→T, common in human population, may exaggerate the adverse effects of ethanol on the brain. | 23118224
 |