FGF ligands of the postnatal mammary stroma regulate distinct aspects of epithelial morphogenesis.
Zhang, X; Martinez, D; Koledova, Z; Qiao, G; Streuli, CH; Lu, P
Development (Cambridge, England)
141
3352-62
2014
Show Abstract
FGF signaling is essential for mammary gland development, yet the mechanisms by which different members of the FGF family control stem cell function and epithelial morphogenesis in this tissue are not well understood. Here, we have examined the requirement of Fgfr2 in mouse mammary gland morphogenesis using a postnatal organ regeneration model. We found that tissue regeneration from basal stem cells is a multistep event, including luminal differentiation and subsequent epithelial branching morphogenesis. Basal cells lacking Fgfr2 did not generate an epithelial network owing to a failure in luminal differentiation. Moreover, Fgfr2 null epithelium was unable to undergo ductal branch initiation and elongation due to a deficiency in directional migration. We identified FGF10 and FGF2 as stromal ligands that control distinct aspects of mammary ductal branching. FGF10 regulates branch initiation, which depends on directional epithelial migration. By contrast, FGF2 controls ductal elongation, requiring cell proliferation and epithelial expansion. Together, our data highlight a pleiotropic role of Fgfr2 in stem cell differentiation and branch initiation, and reveal that different FGF ligands regulate distinct aspects of epithelial behavior. | 25078648
 |
Transplantation of human umbilical mesenchymal stem cells cures the corneal defects of mucopolysaccharidosis VII mice.
Coulson-Thomas, VJ; Caterson, B; Kao, WW
Stem cells (Dayton, Ohio)
31
2116-26
2013
Show Abstract
Mucopolysaccharidosis (MPS) are a family of related disorders caused by a mutation in one of the lysosomal exoglycosidases which leads to the accumulation of glycosaminoglycans (GAGs). MPS VII, caused by a mutation in β-glucuronidase, manifests hepatomegaly, skeletal dysplasia, short stature, corneal clouding, and developmental delay. Current treatment regimens for MPS are not effective for treating corneal clouding and impaired mental development. We hypothesized that human umbilical mesenchymal stem cells (UMSCs) transplanted into the corneal stroma could participate in the catabolism of GAGs providing a means of cell therapy for MPS. For such treatment, human UMSCs were intrastromally transplanted into corneas of MPS VII mice. UMSC transplantation restored the dendritic and hexagonal morphology of host keratocytes and endothelial cells, respectively, and in vivo confocal microscopy (HRT-II) revealed reduced corneal haze. Immunohistochemistry using antibodies against heparan sulfate and chondroitin sulfate chains as well as lysosomal-associated membrane protein 2 revealed a decrease in GAG content and both lysosomal number and size in the treated corneas. Labeling UMSC intracellular compartments prior to transplantation revealed the distribution of UMSC vesicles throughout the corneal stroma and endothelium. An in vitro coculture assay between skin fibroblasts isolated from MPS VII mice and UMSC demonstrated that neutral vesicles released by the UMSC are taken up by the fibroblasts and proceed to fuse with the acidic lysosomes. Therefore, transplanted UMSCs participate both in extracellular GAG turnover and enable host keratocytes to catabolize accumulated GAG products, suggesting that UMSC could be a novel alternative for treating corneal defects associated with MPS and other congenital metabolic disorders. | 23897660
 |
Patient-specific iPSC-derived photoreceptor precursor cells as a means to investigate retinitis pigmentosa.
Tucker, BA; Mullins, RF; Streb, LM; Anfinson, K; Eyestone, ME; Kaalberg, E; Riker, MJ; Drack, AV; Braun, TA; Stone, EM
eLife
2
e00824
2013
Show Abstract
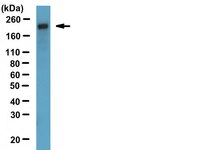
Next-generation and Sanger sequencing were combined to identify disease-causing USH2A mutations in an adult patient with autosomal recessive RP. Induced pluripotent stem cells (iPSCs), generated from the patient's keratinocytes, were differentiated into multi-layer eyecup-like structures with features of human retinal precursor cells. The inner layer of the eyecups contained photoreceptor precursor cells that expressed photoreceptor markers and exhibited axonemes and basal bodies characteristic of outer segments. Analysis of the USH2A transcripts of these cells revealed that one of the patient's mutations causes exonification of intron 40, a translation frameshift and a premature stop codon. Western blotting revealed upregulation of GRP78 and GRP94, suggesting that the patient's other USH2A variant (Arg4192His) causes disease through protein misfolding and ER stress. Transplantation into 4-day-old immunodeficient Crb1 (-/-) mice resulted in the formation of morphologically and immunohistochemically recognizable photoreceptor cells, suggesting that the mutations in this patient act via post-developmental photoreceptor degeneration. DOI:http://dx.doi.org/10.7554/eLife.00824.001. | 23991284
 |