The senescent methylome and its relationship with cancer, ageing and germline genetic variation in humans.
Lowe, R; Overhoff, MG; Ramagopalan, SV; Garbe, JC; Koh, J; Stampfer, MR; Beach, DH; Rakyan, VK; Bishop, CL
Genome biology
16
194
2015
Show Abstract
Cellular senescence is a stable arrest of proliferation and is considered a key component of processes associated with carcinogenesis and other ageing-related phenotypes. Here, we perform methylome analysis of actively dividing and deeply senescent normal human epithelial cells.We identify senescence-associated differentially methylated positions (senDMPs) from multiple experiments using cells from one donor. We find that human senDMP epigenetic signatures are positively and significantly correlated with both cancer and ageing-associated methylation dynamics. We also identify germline genetic variants, including those associated with the p16INK4A locus, which are associated with the presence of in vivo senDMP signatures. Importantly, we also demonstrate that a single senDMP signature can be effectively reversed in a newly-developed protocol of transient senescence reversal.The senDMP signature has significant potential for understanding some of the key (epi)genetic etiological factors that may lead to cancer and age-related diseases in humans. | | 26381124
 |
Expression of the genetic suppressor element 24.2 (GSE24.2) decreases DNA damage and oxidative stress in X-linked dyskeratosis congenita cells.
Manguan-Garcia, C; Pintado-Berninches, L; Carrillo, J; Machado-Pinilla, R; Sastre, L; Pérez-Quilis, C; Esmoris, I; Gimeno, A; García-Giménez, JL; Pallardó, FV; Perona, R
PloS one
9
e101424
2014
Show Abstract
The predominant X-linked form of Dyskeratosis congenita results from mutations in DKC1, which encodes dyskerin, a protein required for ribosomal RNA modification that is also a component of the telomerase complex. We have previously found that expression of an internal fragment of dyskerin (GSE24.2) rescues telomerase activity in X-linked dyskeratosis congenita (X-DC) patient cells. Here we have found that an increased basal and induced DNA damage response occurred in X-DC cells in comparison with normal cells. DNA damage that is also localized in telomeres results in increased heterochromatin formation and senescence. Expression of a cDNA coding for GSE24.2 rescues both global and telomeric DNA damage. Furthermore, transfection of bacterial purified or a chemically synthesized GSE24.2 peptide is able to rescue basal DNA damage in X-DC cells. We have also observed an increase in oxidative stress in X-DC cells and expression of GSE24.2 was able to diminish it. Altogether our data indicated that supplying GSE24.2, either from a cDNA vector or as a peptide reduces the pathogenic effects of Dkc1 mutations and suggests a novel therapeutic approach. | | 24987982
 |
A novel retro-inverso peptide inhibitor reduces amyloid deposition, oxidation and inflammation and stimulates neurogenesis in the APPswe/PS1ΔE9 mouse model of Alzheimer's disease.
Parthsarathy, V; McClean, PL; Hölscher, C; Taylor, M; Tinker, C; Jones, G; Kolosov, O; Salvati, E; Gregori, M; Masserini, M; Allsop, D
PloS one
8
e54769
2013
Show Abstract
Previously, we have developed a retro-inverso peptide inhibitor (RI-OR2, rGffvlkGr) that blocks the in vitro formation and toxicity of the Aβ oligomers which are thought to be a cause of neurodegeneration and memory loss in Alzheimer's disease. We have now attached a retro-inverted version of the HIV protein transduction domain 'TAT' to RI-OR2 to target this new inhibitor (RI-OR2-TAT, Ac-rGffvlkGrrrrqrrkkrGy-NH(2)) into the brain. Following its peripheral injection, a fluorescein-labelled version of RI-OR2-TAT was found to cross the blood brain barrier and bind to the amyloid plaques and activated microglial cells present in the cerebral cortex of 17-months-old APPswe/PS1ΔE9 transgenic mice. Daily intraperitoneal injection of RI-OR2-TAT (at 100 nmol/kg) for 21 days into 10-months-old APPswe/PS1ΔE9 mice resulted in a 25% reduction (pless than 0.01) in the cerebral cortex of Aβ oligomer levels, a 32% reduction (pless than 0.0001) of β-amyloid plaque count, a 44% reduction (pless than 0.0001) in the numbers of activated microglial cells, and a 25% reduction (pless than 0.0001) in oxidative damage, while the number of young neurons in the dentate gyrus was increased by 210% (pless than 0.0001), all compared to control APPswe/PS1ΔE9 mice injected with vehicle (saline) alone. Our data suggest that oxidative damage, inflammation, and inhibition of neurogenesis are all a downstream consequence of Aβ aggregation, and identify a novel brain-penetrant retro-inverso peptide inhibitor of Aβ oligomer formation for further testing in humans as a potential disease-modifying treatment for Alzheimer's disease. | | 23382963
 |
NADPH oxidase mediates striatal neuronal injury after transient global cerebral ischemia.
Yoshioka, H; Niizuma, K; Katsu, M; Okami, N; Sakata, H; Kim, GS; Narasimhan, P; Chan, PH
Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism
31
868-80
2011
Show Abstract
Medium spiny neurons (MSNs) constitute most of the striatal neurons and are known to be vulnerable to ischemia; however, the mechanisms of the vulnerability remain unclear. Activated forms of nicotinamide-adenine dinucleotide phosphate (NADPH) oxidase (NOX), which require interaction between cytosolic and membrane-bound subunits, are among the major sources of superoxide in the central nervous system. Although increasing evidence suggests that NOX has important roles in neurodegenerative diseases, its roles in MSN injury after transient global cerebral ischemia (tGCI) have not been elucidated. To clarify this issue, C57BL/6 mice were subjected to tGCI by bilateral common carotid artery occlusion for 22 minutes. Western blot analysis revealed upregulation of NOX subunits and recruitment of cytosolic subunits to the cell membrane at early (3 to 6 hours) and late (72 hours) phases after tGCI. Taken together with immunofluorescent studies, this activation arose in MSNs and endothelial cells at the early phase, and in reactive microglia at the late phase. Pharmacological and genetic inhibition of NOX attenuated oxidative injury, microglial activation, and MSN death after tGCI. These findings suggest that NOX has pivotal roles in MSN injury after tGCI and could be a therapeutic target for brain ischemia. Full Text Article | | 20859296
 |
Consistent injury to medium spiny neurons and white matter in the mouse striatum after prolonged transient global cerebral ischemia.
Yoshioka, H; Niizuma, K; Katsu, M; Sakata, H; Okami, N; Chan, PH
Journal of neurotrauma
28
649-60
2011
Show Abstract
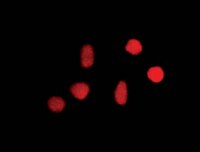
A reproducible transient global cerebral ischemia (tGCI) mouse model has not been fully established. Although striatal neurons and white matter are recognized to be vulnerable to ischemia, their injury after tGCI in mice has not been elucidated. The purpose of this study was to evaluate injuries to striatal neurons and white matter after tGCI in C57BL/6 mice, and to develop a reproducible tGCI model. Male C57BL/6 mice were subjected to tGCI by bilateral common carotid artery occlusion (BCCAO). Mice whose cortical cerebral blood flow after BCCAO decreased to less than 13% of the pre-ischemic value were used. Histological analysis showed that at 3 days after 22 min of BCCAO, striatal neurons were injured more consistently than those in other brain regions. Quantitative analysis of cytochrome c release into the cytosol and DNA fragmentation in the striatum showed consistent injury to the striatum. Immunohistochemistry and Western blot analysis revealed that DARPP-32-positive medium spiny neurons, the majority of striatal neurons, were the most vulnerable among the striatal neuronal subpopulations. The striatum (especially medium spiny neurons) was susceptible to oxidative stress after tGCI, which is probably one of the mechanisms of vulnerability. SMI-32 immunostaining showed that white matter in the striatum was also consistently injured 3 days after 22 min of BCCAO. We thus suggest that this is a tGCI model using C57BL/6 mice that consistently produces neuronal and white matter injury in the striatum by a simple technique. This model can be highly applicable for elucidating molecular mechanisms in the brain after global ischemia. | Immunofluorescence | 21309724
 |
Mitochondrial DNA toxicity compromises mitochondrial dynamics and induces hippocampal antioxidant defenses.
Lauritzen, KH; Cheng, C; Wiksen, H; Bergersen, LH; Klungland, A
DNA repair
10
639-53
2011
Show Abstract
Mitochondria are highly dynamic organelles that can be actively transported within the cell to satisfy local requirements. They are vital for providing cellular energy, but are also an important endogenous source of reactive oxygen species. The distribution of mitochondria is particularly important for neurons because of the morphological complexity of these cells, and because neural processing is metabolically expensive. Defects in mitochondrial distribution, observed in several neurodegenerative diseases, can result in synaptic dysfunction. We have generated transgenic mice expressing an enzyme in forebrain neurons that causes mitochondrial DNA (mtDNA) damage in the form of abasic-sites, creating mtDNA toxicity. Here, we report that mitochondrial distribution is disturbed in hippocampal neurons of these mice. Moreover, mtDNA copy number and mitochondrial transcription are reduced, and oxidative stress is increased. There is also a loss of receptors at excitatory glutamatergic synapses in the dentate gyrus, and the size of the postsynaptic density in this region is abnormal. We speculate that the loss of synaptic mitochondria caused by accumulation in the neuronal cell body contributes to the observed synaptic abnormalities, as well as the overall loss of mtDNA and diminished mitochondrial transcription. Collectively, these changes lead to mitochondria with reduced function and increased oxidative stress. | | 21550321
 |
Adding insult to injury: effects of xenobiotic-induced preantral ovotoxicity on ovarian development and oocyte fusibility.
Sobinoff, AP; Pye, V; Nixon, B; Roman, SD; McLaughlin, EA
Toxicological sciences : an official journal of the Society of Toxicology
118
653-66
2010
Show Abstract
Mammalian females are born with a finite number of nonrenewing primordial follicles, the majority of which remain in a quiescent state for many years. Because of their nonrenewing nature, these "resting" oocytes are particularly vulnerable to xenobiotic insult, resulting in premature ovarian senescence and the formation of dysfunctional oocytes. In this study, we characterized the mechanisms of ovotoxicity for three ovotoxic agents, 4-vinylcyclohexene diepoxide (VCD), methoxychlor (MXC), and menadione (MEN), all of which target immature follicles. Microarray analysis of neonatal mouse ovaries exposed to these xenobiotics in vitro revealed a more than twofold significant difference in transcript expression (p less than 0.05) for a number of genes associated with apoptotic cell death and primordial follicle activation. Histomorphological and immunohistological analysis supported the microarray data, showing signs of primordial follicle activation and preantral follicle atresia both in vitro and in vivo. Sperm-oocyte fusion assays on oocytes obtained from adult Swiss mice treated neonatally revealed severely reduced sperm-egg binding and fusion in a dose-dependent manner for all the xenobiotic treatments. Additionally, lipid peroxidation analysis on xenobiotic-cultured oocytes indicated a dose-dependent increase in oocyte lipid peroxidation for all three xenobiotics in vitro. Our results reveal a novel mechanism of preantral ovotoxicity involving the homeostatic recruitment of primordial follicles to maintain the pool of developing follicles destroyed by xenobiotic exposure and to our knowledge provide the first documented evidence of short-term, low- and high-dose (VCD 40-80 mg/kg/day, MXC 50-100 mg/kg/day, MEN 7.5-15 mg/kg/day) neonatal exposure to xenobiotics causing long-term reactive oxygen species-induced oocyte dysfunction. | | 20829426
 |
Trypanosoma cruzi induces the reactive oxygen species-PARP-1-RelA pathway for up-regulation of cytokine expression in cardiomyocytes.
Ba, X; Gupta, S; Davidson, M; Garg, NJ
The Journal of biological chemistry
285
11596-606
2010
Show Abstract
In this study, we demonstrate that human cardiomyocytes (AC16) produce reactive oxygen species (ROS) and inflammatory cytokines in response to Trypanosoma cruzi. ROS were primarily produced by mitochondria, some of which diffused to cytosol of infected cardiomyocytes. These ROS resulted in an increase in 8-hydroxyguanine lesions and DNA fragmentation that signaled PARP-1 activation evidenced by poly(ADP-ribose) (PAR) modification of PARP-1 and other proteins in infected cardiomyocytes. Phenyl-alpha-tert-butylnitrone blocked the mitochondrial ROS (mtROS) formation, DNA damage, and PARP-1 activation in infected cardiomyocytes. Further inhibition studies demonstrated that ROS and PARP-1 signaled TNF-alpha and IL-1beta expression in infected cardiomyocytes. ROS directly signaled the nuclear translocation of RelA (p65), NF-kappaB activation, and cytokine gene expression. PARP-1 exhibited no direct interaction with p65 and did not signal its translocation to nuclei in infected cardiomyocytes. Instead, PARP-1 contributed to PAR modification of p65-interacting nuclear proteins and assembly of the NF-kappaB transcription complex. PJ34 (PARP-1 inhibitor) also prevented mitochondrial poly(ADP-ribosyl)ation (PARylation) and ROS formation. We conclude that T. cruzi-mediated mtROS provide primary stimulus for PARP-1-NF-kappaB activation and cytokine gene expression in infected cardiomyocytes. PAR modification of mitochondrial membranes then results in a feedback cycle of mtROS formation and DNA damage/PARP-1 activation. ROS, either through direct modulation of cytosolic NF-kappaB, or via PARP-1-dependent PAR modification of p65-interacting nuclear proteins, contributes to cytokine gene expression. Our results demonstrate a link between ROS and inflammatory responses in cardiomyocytes infected by T. cruzi and provide a clue to the pathomechanism of sustained inflammation in Chagas disease. Full Text Article | | 20145242
 |
Vascular effects of a low-carbohydrate high-protein diet.
Foo, SY; Heller, ER; Wykrzykowska, J; Sullivan, CJ; Manning-Tobin, JJ; Moore, KJ; Gerszten, RE; Rosenzweig, A
Proceedings of the National Academy of Sciences of the United States of America
106
15418-23
2009
Show Abstract
The cardiovascular complications of obesity have prompted interest in dietary interventions to reduce weight, including low-carbohydrate diets that are generally high in protein and fat. However, little is known about the long-term effects of these diets on vascular health. We examined the cardiovascular effects of a low-carbohydrate, high-protein diet (LCHP) in the ApoE(-/-) mouse model of atherosclerosis and in a model of ischemia-induced neovascularization. Mice on a LCHP were compared with mice maintained on either the standard chow diet (SC) or the Western diet (WD) which contains comparable fat and cholesterol to the LCHP. LCHP-fed mice developed more aortic atherosclerosis and had an impaired ability to generate new vessels in response to tissue ischemia. These changes were not explained by alterations in serum cholesterol, inflammatory mediators or infiltrates, or oxidative stress. The LCHP diet substantially reduced the number of bone marrow and peripheral blood endothelial progenitor cells (EPCs), a marker of vascular regenerative capacity. EPCs from mice on a LCHP diet also manifest lower levels of activated (phosphorylated) Akt, a serine-threonine kinase important in EPC mobilization, proliferation, and survival. Taken together, these data demonstrate that in animal models LCHP diets have adverse vascular effects not reflected in serum markers and that nonlipid macronutrients can modulate vascular progenitor cells and pathophysiology. | | 19706393
 |
The JmjC domain histone demethylase Ndy1 regulates redox homeostasis and protects cells from oxidative stress.
Polytarchou, C; Pfau, R; Hatziapostolou, M; Tsichlis, PN
Molecular and cellular biology
28
7451-64
2008
Show Abstract
The histone H3 demethylase Ndy1/KDM2B protects cells from replicative senescence. Changes in the metabolism of reactive oxygen species (ROS) are important for establishing senescence, suggesting that Ndy1 may play a role in redox regulation. Here we show that Ndy1 protects from H(2)O(2)-induced apoptosis and G(2)/M arrest and inhibits ROS-mediated signaling and DNA damage, while knockdown of Ndy1 has the opposite effects. Consistent with these observations, whereas Ndy1 overexpression promotes H(2)O(2) detoxification, Ndy1 knockdown inhibits it. Ndy1 promotes the expression of genes encoding the antioxidant enzymes aminoadipic semialdehyde synthase (Aass), NAD(P)H quinone oxidoreductase-1 (Nqo1), peroxiredoxin-4 (Prdx4), and serine peptidase inhibitor b1b (Serpinb1b) and represses the expression of interleukin-19. At least two of these genes (Nqo1 and Prdx4) are regulated directly by Ndy1, which binds to specific sites within their promoters and demethylates promoter-associated histone H3 dimethylated at K36 and histone H3 trimethylated at K4. Simultaneous knockdown of Aass, Nqo1, Prdx4, and Serpinb1b in Ndy1-expressing cells to levels equivalent to those detected in control cells was sufficient to suppress the Ndy1 redox phenotype. | Western Blotting | 18838535
 |