Interleukin-22 is increased in multiple sclerosis patients and targets astrocytes.
Perriard, G; Mathias, A; Enz, L; Canales, M; Schluep, M; Gentner, M; Schaeren-Wiemers, N; Du Pasquier, RA
Journal of neuroinflammation
12
119
2015
Show Abstract
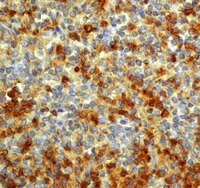
Increasing evidences link T helper 17 (Th17) cells with multiple sclerosis (MS). In this context, interleukin-22 (IL-22), a Th17-linked cytokine, has been implicated in blood brain barrier breakdown and lymphocyte infiltration. Furthermore, polymorphism between MS patients and controls has been recently described in the gene coding for IL-22 binding protein (IL-22BP). Here, we aimed to better characterize IL-22 in the context of MS.IL-22 and IL-22BP expressions were assessed by ELISA and qPCR in the following compartments of MS patients and control subjects: (1) the serum, (2) the cerebrospinal fluid, and (3) immune cells of peripheral blood. Identification of the IL-22 receptor subunit, IL-22R1, was performed by immunohistochemistry and immunofluorescence in human brain tissues and human primary astrocytes. The role of IL-22 on human primary astrocytes was evaluated using 7-AAD and annexin V, markers of cell viability and apoptosis, respectively.In a cohort of 141 MS patients and healthy control (HC) subjects, we found that serum levels of IL-22 were significantly higher in relapsing MS patients than in HC but also remitting and progressive MS patients. Monocytes and monocyte-derived dendritic cells contained an enhanced expression of mRNA coding for IL-22BP as compared to HC. Using immunohistochemistry and confocal microscopy, we found that IL-22 and its receptor were detected on astrocytes of brain tissues from both control subjects and MS patients, although in the latter, the expression was higher around blood vessels and in MS plaques. Cytometry-based functional assays revealed that addition of IL-22 improved the survival of human primary astrocytes. Furthermore, tumor necrosis factor α-treated astrocytes had a better long-term survival capacity upon IL-22 co-treatment. This protective effect of IL-22 seemed to be conferred, at least partially, by a decreased apoptosis.We show that (1) there is a dysregulation in the expression of IL-22 and its antagonist, IL-22BP, in MS patients, (2) IL-22 targets specifically astrocytes in the human brain, and (3) this cytokine confers an increased survival of the latter cells. | | | 26077779
 |
A hyaluronan-based scaffold for the in vitro construction of dental pulp-like tissue.
Ferroni, L; Gardin, C; Sivolella, S; Brunello, G; Berengo, M; Piattelli, A; Bressan, E; Zavan, B
International journal of molecular sciences
16
4666-81
2015
Show Abstract
Dental pulp tissue supports the vitality of the tooth, but it is particularly vulnerable to external insults, such as mechanical trauma, chemical irritation or microbial invasion, which can lead to tissue necrosis. In the present work, we present an endodontic regeneration method based on the use of a tridimensional (3D) hyaluronan scaffold and human dental pulp stem cells (DPSCs) to produce a functional dental pulp-like tissue in vitro. An enriched population of DPSCs was seeded onto hyaluronan-based non-woven meshes in the presence of differentiation factors to induce the commitment of stem cells to neuronal, glial, endothelial and osteogenic phenotypes. In vitro experiments, among which were gene expression profiling and immunofluorescence (IF) staining, proved the commitment of DPSCs to the main components of dental pulp tissue. In particular, the hyaluronan-DPSCs construct showed a dental pulp-like morphology consisting of several specialized cells growing inside the hyaluronan fibers. Furthermore, these constructs were implanted into rat calvarial critical-size defects. Histological analyses and gene expression profiling performed on hyaluronan-DPSCs grafts showed the regeneration of osteodentin-like tissue. Altogether, these data suggest the regenerative potential of the hyaluronan-DPSC engineered tissue. | | | 25739081
 |
Periostin Promotes Neural Stem Cell Proliferation and Differentiation following Hypoxic-Ischemic Injury.
Ma, SM; Chen, LX; Lin, YF; Yan, H; Lv, JW; Xiong, M; Li, J; Cheng, GQ; Yang, Y; Qiu, ZL; Zhou, WH
PloS one
10
e0123585
2015
Show Abstract
Neural stem cell (NSC) proliferation and differentiation are required to replace neurons damaged or lost after hypoxic-ischemic events and recover brain function. Periostin (POSTN), a novel matricellular protein, plays pivotal roles in the survival, migration, and regeneration of various cell types, but its function in NSCs of neonatal rodent brain is still unknown. The purpose of this study was to investigate the role of POSTN in NSCs following hypoxia-ischemia (HI). We found that POSTN mRNA levels significantly increased in differentiating NSCs. The proliferation and differentiation of NSCs in the hippocampus is compromised in POSTN knockout mice. Moreover, NSC proliferation and differentiation into neurons and astrocytes significantly increased in cultured NSCs treated with recombinant POSTN. Consistently, injection of POSTN into neonatal hypoxic-ischemic rat brains stimulated NSC proliferation and differentiation in the subventricular and subgranular zones after 7 and 14 days of brain injury. Lastly, POSTN treatment significantly improved the spatial learning deficits of rats subjected to HI. These results suggest that POSTN significantly enhances NSC proliferation and differentiation after HI, and provides new insights into therapeutic strategies for the treatment of hypoxic-ischemic encephalopathy. | | | 25894199
 |
Neuroprotective effects of oligodendrocyte progenitor cell transplantation in premature rat brain following hypoxic-ischemic injury.
Chen, LX; Ma, SM; Zhang, P; Fan, ZC; Xiong, M; Cheng, GQ; Yang, Y; Qiu, ZL; Zhou, WH; Li, J
PloS one
10
e0115997
2015
Show Abstract
Periventricular leukomalacia (PVL) is a common ischemic brain injury in premature infants for which there is no effective treatment. The objective of this study was to determine whether transplanted mouse oligodendrocyte progenitor cells (OPCs) have neuroprotective effects in a rat model of PVL. Hypoxia-ischemia (HI) was induced in 3-day-old rat pups by left carotid artery ligation, followed by exposure to 6% oxygen for 2.5 h. Animals were assigned to OPC transplantation or sham control groups and injected with OPCs or PBS, respectively, and sacrificed up to 6 weeks later for immunohistochemical analysis to investigate the survival and differentiation of transplanted OPCs. Apoptosis was evaluated by double immunolabeling of brain sections for caspase-3 and neuronal nuclei (NeuN), while proliferation was assessed using a combination of anti-Nestin and -bromodeoxyuridine antibodies. The expression of brain-derived neurotrophic factor (BDNF) and Bcl-2 was examined 7 days after OPC transplantation. The Morris water maze was used to test spatial learning and memory. The results showed that transplanted OPCs survived and formed a myelin sheath, and stimulated BDNF and Bcl-2 expression and the proliferation of neural stem cells (NSC), while inhibiting HI-induced neuronal apoptosis relative to control animals. Moreover, deficits in spatial learning and memory resulting from HI were improved by OPC transplantation. These results demonstrate an important neuroprotective role for OPCs that can potentially be exploited in cell-based therapeutic approaches to minimize HI-induced brain injury. | | | 25790286
 |
The serine protease inhibitor SerpinA3N attenuates neuropathic pain by inhibiting T cell-derived leukocyte elastase.
Vicuña, L; Strochlic, DE; Latremoliere, A; Bali, KK; Simonetti, M; Husainie, D; Prokosch, S; Riva, P; Griffin, RS; Njoo, C; Gehrig, S; Mall, MA; Arnold, B; Devor, M; Woolf, CJ; Liberles, SD; Costigan, M; Kuner, R
Nature medicine
21
518-23
2015
Show Abstract
Neuropathic pain is a major, intractable clinical problem and its pathophysiology is not well understood. Although recent gene expression profiling studies have enabled the identification of novel targets for pain therapy, classical study designs provide unclear results owing to the differential expression of hundreds of genes across sham and nerve-injured groups, which can be difficult to validate, particularly with respect to the specificity of pain modulation. To circumvent this, we used two outbred lines of rats, which are genetically similar except for being genetically segregated as a result of selective breeding for differences in neuropathic pain hypersensitivity. SerpinA3N, a serine protease inhibitor, was upregulated in the dorsal root ganglia (DRG) after nerve injury, which was further validated for its mouse homolog. Mice lacking SerpinA3N developed more neuropathic mechanical allodynia than wild-type (WT) mice, and exogenous delivery of SerpinA3N attenuated mechanical allodynia in WT mice. T lymphocytes infiltrate the DRG after nerve injury and release leukocyte elastase (LE), which was inhibited by SerpinA3N derived from DRG neurons. Genetic loss of LE or exogenous application of a LE inhibitor (Sivelastat) in WT mice attenuated neuropathic mechanical allodynia. Overall, we reveal a novel and clinically relevant role for a member of the serpin superfamily and a leukocyte elastase and crosstalk between neurons and T cells in the modulation of neuropathic pain. | | | 25915831
 |
A BMP7 Variant Inhibits Tumor Angiogenesis In Vitro and In Vivo through Direct Modulation of Endothelial Cell Biology.
Tate, CM; Mc Entire, J; Pallini, R; Vakana, E; Wyss, L; Blosser, W; Ricci-Vitiani, L; D'Alessandris, QG; Morgante, L; Giannetti, S; Larocca, LM; Todaro, M; Benfante, A; Colorito, ML; Stassi, G; De Maria, R; Rowlinson, S; Stancato, L
PloS one
10
e0125697
2015
Show Abstract
Bone morphogenetic proteins (BMPs), members of the TGF-β superfamily, have numerous biological activities including control of growth, differentiation, and vascular development. Using an in vitro co-culture endothelial cord formation assay, we investigated the role of a BMP7 variant (BMP7v) in VEGF, bFGF, and tumor-driven angiogenesis. BMP7v treatment led to disruption of neo-endothelial cord formation and regression of existing VEGF and bFGF cords in vitro. Using a series of tumor cell models capable of driving angiogenesis in vitro, BMP7v treatment completely blocked cord formation. Pre-treatment of endothelial cells with BMP7v significantly reduced their cord forming ability, indicating a direct effect on endothelial cell function. BMP7v activated the canonical SMAD signaling pathway in endothelial cells but targeted gene knockdown using shRNA directed against SMAD4 suggests this pathway is not required to mediate the anti-angiogenic effect. In contrast to SMAD activation, BMP7v selectively decreased ERK and AKT activation, significantly decreased endothelial cell migration and down-regulated expression of critical RTKs involved in VEGF and FGF angiogenic signaling, VEGFR2 and FGFR1 respectively. Importantly, in an in vivo angiogenic plug assay that serves as a measurement of angiogenesis, BMP7v significantly decreased hemoglobin content indicating inhibition of neoangiogenesis. In addition, BMP7v significantly decreased angiogenesis in glioblastoma stem-like cell (GSLC) Matrigel plugs and significantly impaired in vivo growth of a GSLC xenograft with a concomitant reduction in microvessel density. These data support BMP7v as a potent anti-angiogenic molecule that is effective in the context of tumor angiogenesis. | | | 25919028
 |
Profilin isoforms modulate astrocytic morphology and the motility of astrocytic processes.
Schweinhuber, SK; Meßerschmidt, T; Hänsch, R; Korte, M; Rothkegel, M
PloS one
10
e0117244
2015
Show Abstract
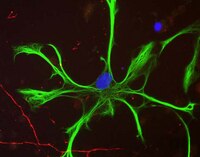
The morphology of astrocytic processes determines their close structural association with synapses referred to as the 'tripartite synapse'. Concerted morphological plasticity processes at tripartite synapses are supposed to shape neuronal communication. Morphological changes in astrocytes as well as the motility of astrocytic processes require remodeling of the actin cytoskeleton. Among the regulators of fast timescale actin-based motility, the actin binding protein profilin 1 has recently been shown to control the activity-dependent outgrowth of astrocytic processes. Here, we demonstrate that cultured murine astrocytes in addition to the ubiquitous profilin 1 also express the neuronal isoform profilin 2a. To analyze the cellular function of both profilins in astrocytes, we took advantage of a shRNA mediated isoform-specific downregulation. Interestingly, consistent with earlier results in neurons, we found redundant as well as isoform-specific functions of both profilins in modulating cellular physiology. The knockdown of either profilin 1 or profilin 2a led to a significant decrease in cell spreading of astrocytes. In contrast, solely the knockdown of profilin 2a resulted in a significantly reduced morphological complexity of astrocytes in both dissociated and slice culture astrocytes. Moreover, both isoforms proved to be crucial for forskolin-induced astrocytic stellation. Furthermore, forskolin treatment resulted in isoform-specific changes in the phosphorylation level of profilin 1 and profilin 2a, leading to a PKA-dependent phosphorylation of profilin 2a. In addition, transwell assays revealed an involvement of both isoforms in the motility of astrocytic processes, while FRAP analysis displayed an isoform-specific role of profilin 1 in the regulation of actin dynamics in peripheral astrocytic processes. Taken together, we suggest profilin isoforms to be important modulators of astrocytic morphology and motility with overlapping as well as isoform-specific functions. | | | 25629407
 |
Cortical neurons are a prominent source of the proinflammatory cytokine osteopontin in HIV-associated neurocognitive disorders.
Silva, K; Hope-Lucas, C; White, T; Hairston, TK; Rameau, T; Brown, A
Journal of neurovirology
21
174-85
2015
Show Abstract
The proinflammatory cytokine osteopontin (OPN) is elevated in the cerebrospinal fluid (CSF) in individuals with HIV-associated neurocognitive disorders (HAND) and remains so in those on suppressive antiretroviral therapy. To understand the pathophysiological significance of elevated OPN in the CNS, we sought to determine the cellular source of this cytokine. As HIV-1 replicates productively in macrophages/microglia, we tested whether these cells are the predominant producers of OPN in the brain. Stringent patient selection criteria, which excluded brain tissues from those with evidence of drug abuse and dependence, were used. Uninfected normal controls, amyotrophic lateral sclerosis (ALS), HIV+ asymptomatic neurocognitive impairment (ANI), and HIV+ mild neurocognitive disorder (MND)/HIV-associated dementia (HAD) groups were included. Double-label immunohistochemistry for CNS cells and OPN was used to quantify OPN expression in astrocytes, macrophages/microglia, and neurons. While resident macrophages/microglia expressed OPN, astrocytes and unexpectedly neurons were also a major source of OPN. OPN levels in ionized Ca(2+)-binding adapter 1 (Iba1)/allograft inflammatory factor-1 (AIF-1)+ microglia in HIV+ ANI and MND/HAD exceeded those of HIV-negative controls and were comparable to expression seen in ALS. Moreover, in neurons, OPN was expressed at the highest levels in the HIV+ ANI group. These findings suggest that while infiltrating HIV-infected macrophages are most likely the initial source of OPN, resident CNS cells become activated and also express this inflammatory cytokine at significant levels. Moreover, as OPN levels are elevated compared to uninfected individuals and increases with the severity of impairment, it appears that the expression of OPN is persistent and sustained within the brain parenchyma in those that progress to HAND. | | | 25636782
 |
dNP2 is a blood-brain barrier-permeable peptide enabling ctCTLA-4 protein delivery to ameliorate experimental autoimmune encephalomyelitis.
Lim, S; Kim, WJ; Kim, YH; Lee, S; Koo, JH; Lee, JA; Yoon, H; Kim, DH; Park, HJ; Kim, HM; Lee, HG; Yun Kim, J; Lee, JU; Hun Shin, J; Kyun Kim, L; Doh, J; Kim, H; Lee, SK; Bothwell, AL; Suh, M; Choi, JM
Nature communications
6
8244
2015
Show Abstract
Central nervous system (CNS)-infiltrating effector T cells play critical roles in the development and progression of multiple sclerosis (MS). However, current drugs for MS are very limited due to the difficulty of delivering drugs into the CNS. Here we identify a cell-permeable peptide, dNP2, which efficiently delivers proteins into mouse and human T cells, as well as various tissues. Moreover, it enters the brain tissue and resident cells through blood vessels by penetrating the tightly organized blood-brain barrier. The dNP2-conjugated cytoplasmic domain of cytotoxic T-lymphocyte antigen 4 (dNP2-ctCTLA-4) negatively regulates activated T cells and shows inhibitory effects on experimental autoimmune encephalomyelitis in both preventive and therapeutic mouse models, resulting in the reduction of demyelination and CNS-infiltrating T helper 1 and T helper 17 cells. Thus, this study demonstrates that dNP2 is a blood-brain barrier-permeable peptide and dNP2-ctCTLA-4 could be an effective agent for treating CNS inflammatory diseases such as MS. | | | 26372309
 |
Delayed progesterone treatment reduces brain infarction and improves functional outcomes after ischemic stroke: a time-window study in middle-aged rats.
Yousuf, S; Sayeed, I; Atif, F; Tang, H; Wang, J; Stein, DG
Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism
34
297-306
2014
Show Abstract
We evaluated the neuroprotective effects of delayed progesterone (PROG) treatment against ischemic stroke-induced neuronal death, inflammation, and functional deficits. We induced transient focal cerebral ischemia in male rats and administered PROG (8 mg/kg) or vehicle intraperitoneally at 3, 6, or 24 hours post occlusion, subcutaneously 5 hours later and then every 24 hours for 7 days. Behavioral outcomes were evaluated over 22 days. Infarct size and other biomarkers of injury were evaluated by cresyl violet staining, and matrix metalloproteinase-9 (MMP-9), glial fibrillary acidic protein (GFAP), and vascular endothelial growth factor (VEGF) by immunofluorescence. Progesterone treatment started at 3 and 6 hours post occlusion significantly (Pless than 0.05) improved behavioral performance at all time points (74.01%) and reduced infarction volume (61.68%) compared with vehicle. No significant difference was observed between the 3 and 6 hour PROG treatment groups. Matrix metalloproteinase-9 and VEGF were upregulated in the PROG groups compared with vehicle. Glial fibrillary acidic protein expression was increased in the vehicle group but markedly lower in the PROG groups. Treatment delayed for 24 hours did not significantly improve functional outcomes or reduce infarction volume. We conclude that, under the right treatment conditions, PROG treatment delayed up to 6 hours can improve functional deficits and reduce brain infarction, possibly by modulating GFAP, VEGF, and MMP-9 expression. | | | 24301297
 |