Pharmacologic suppression of JAK1/2 by JAK1/2 inhibitor AZD1480 potently inhibits IL-6-induced experimental prostate cancer metastases formation.
Gu, L; Talati, P; Vogiatzi, P; Romero-Weaver, AL; Abdulghani, J; Liao, Z; Leiby, B; Hoang, DT; Mirtti, T; Alanen, K; Zinda, M; Huszar, D; Nevalainen, MT
Molecular cancer therapeutics
13
1246-58
2014
Show Abstract
Metastatic prostate cancer is lethal and lacks effective strategies for prevention or treatment, requiring novel therapeutic approaches. Interleukin-6 (IL-6) is a cytokine that has been linked with prostate cancer pathogenesis by multiple studies. However, the direct functional roles of IL-6 in prostate cancer growth and progression have been unclear. In the present study, we show that IL-6 is produced in distant metastases of clinical prostate cancers. IL-6-activated signaling pathways in prostate cancer cells induced a robust 7-fold increase in metastases formation in nude mice. We further show that IL-6 promoted migratory prostate cancer cell phenotype, including increased prostate cancer cell migration, microtubule reorganization, and heterotypic adhesion of prostate cancer cells to endothelial cells. IL-6-driven metastasis was predominantly mediated by Stat3 and to lesser extent by ERK1/2. Most importantly, pharmacologic inhibition of Jak1/2 by AZD1480 suppressed IL-6-induced signaling, migratory prostate cancer cell phenotypes, and metastatic dissemination of prostate cancer in vivo in nude mice. In conclusion, we demonstrate that the cytokine IL-6 directly promotes prostate cancer metastasis in vitro and in vivo via Jak-Stat3 signaling pathway, and that IL-6-driven metastasis can be effectively suppressed by pharmacologic targeting of Jak1/2 using Jak1/2 inhibitor AZD1480. Our results therefore provide a strong rationale for further development of Jak1/2 inhibitors as therapy for metastatic prostate cancer. | | | 24577942
 |
Altered translation of GATA1 in Diamond-Blackfan anemia.
Ludwig, LS; Gazda, HT; Eng, JC; Eichhorn, SW; Thiru, P; Ghazvinian, R; George, TI; Gotlib, JR; Beggs, AH; Sieff, CA; Lodish, HF; Lander, ES; Sankaran, VG
Nature medicine
20
748-53
2014
Show Abstract
Ribosomal protein haploinsufficiency occurs in diverse human diseases including Diamond-Blackfan anemia (DBA), congenital asplenia and T cell leukemia. Yet, how mutations in genes encoding ubiquitously expressed proteins such as these result in cell-type- and tissue-specific defects remains unknown. Here, we identify mutations in GATA1, encoding the critical hematopoietic transcription factor GATA-binding protein-1, that reduce levels of full-length GATA1 protein and cause DBA in rare instances. We show that ribosomal protein haploinsufficiency, the more common cause of DBA, can lead to decreased GATA1 mRNA translation, possibly resulting from a higher threshold for initiation of translation of this mRNA in comparison with other mRNAs. In primary hematopoietic cells from patients with mutations in RPS19, encoding ribosomal protein S19, the amplitude of a transcriptional signature of GATA1 target genes was globally and specifically reduced, indicating that the activity, but not the mRNA level, of GATA1 is decreased in patients with DBA associated with mutations affecting ribosomal proteins. Moreover, the defective hematopoiesis observed in patients with DBA associated with ribosomal protein haploinsufficiency could be partially overcome by increasing GATA1 protein levels. Our results provide a paradigm by which selective defects in translation due to mutations affecting ubiquitous ribosomal proteins can result in human disease. | | | 24952648
 |
A novel role for histone deacetylase 6 in the regulation of the tolerogenic STAT3/IL-10 pathway in APCs.
Cheng, F; Lienlaf, M; Wang, HW; Perez-Villarroel, P; Lee, C; Woan, K; Rock-Klotz, J; Sahakian, E; Woods, D; Pinilla-Ibarz, J; Kalin, J; Tao, J; Hancock, W; Kozikowski, A; Seto, E; Villagra, A; Sotomayor, EM
Journal of immunology (Baltimore, Md. : 1950)
193
2850-62
2014
Show Abstract
APCs are critical in T cell activation and in the induction of T cell tolerance. Epigenetic modifications of specific genes in the APC play a key role in this process, and among them histone deacetylases (HDACs) have emerged as key participants. HDAC6, one of the members of this family of enzymes, has been shown to be involved in regulation of inflammatory and immune responses. In this study, to our knowledge we show for the first time that genetic or pharmacologic disruption of HDAC6 in macrophages and dendritic cells results in diminished production of the immunosuppressive cytokine IL-10 and induction of inflammatory APCs that effectively activate Ag-specific naive T cells and restore the responsiveness of anergic CD4(+) T cells. Mechanistically, we have found that HDAC6 forms a previously unknown molecular complex with STAT3, association that was detected in both the cytoplasmic and nuclear compartments of the APC. By using HDAC6 recombinant mutants we identified the domain comprising amino acids 503-840 as being required for HDAC6 interaction with STAT3. Furthermore, by re-chromatin immunoprecipitation we confirmed that HDAC6 and STAT3 are both recruited to the same DNA sequence within the Il10 gene promoter. Of note, disruption of this complex by knocking down HDAC6 resulted in decreased STAT3 phosphorylation--but no changes in STAT3 acetylation--as well as diminished recruitment of STAT3 to the Il10 gene promoter region. The additional demonstration that a selective HDAC6 inhibitor disrupts this STAT3/IL-10 tolerogenic axis points to HDAC6 as a novel molecular target in APCs to overcome immune tolerance and tips the balance toward T cell immunity. | | | 25108026
 |
Tumor suppressor miR-375 regulates MYC expression via repression of CIP2A coding sequence through multiple miRNA-mRNA interactions.
Jung, HM; Patel, RS; Phillips, BL; Wang, H; Cohen, DM; Reinhold, WC; Chang, LJ; Yang, LJ; Chan, EK
Molecular biology of the cell
24
1638-48, S1-7
2013
Show Abstract
MicroRNAs (miRNAs) are small, noncoding RNAs involved in posttranscriptional regulation of protein-coding genes in various biological processes. In our preliminary miRNA microarray analysis, miR-375 was identified as the most underexpressed in human oral tumor versus controls. The purpose of the present study is to examine the function of miR-375 as a candidate tumor suppressor miRNA in oral cancer. Cancerous inhibitor of PP2A (CIP2A), a guardian of oncoprotein MYC, is identified as a candidate miR-375 target based on bioinformatics. Luciferase assay accompanied by target sequence mutagenesis elucidates five functional miR-375-binding sites clustered in the CIP2A coding sequence close to the C-terminal domain. Overexpression of CIP2A is clearly demonstrated in oral cancers, and inverse correlation between miR-375 and CIP2A is observed in the tumors, as well as in NCI-60 cell lines, indicating the potential generalized involvement of the miR-375-CIP2A relationship in many other cancers. Transient transfection of miR-375 in oral cancer cells reduces the expression of CIP2A, resulting in decrease of MYC protein levels and leading to reduced proliferation, colony formation, migration, and invasion. Therefore this study shows that underexpression of tumor suppressor miR-375 could lead to uncontrolled CIP2A expression and extended stability of MYC, which contributes to promoting cancerous phenotypes. | Western Blotting | | 23552692
 |
Identification of a redox-sensitive switch within the JAK2 catalytic domain.
John K Smith,Chetan N Patil,Srikant Patlolla,Barak W Gunter,George W Booz,Roy J Duhé
Free radical biology & medicine
52
2012
Show Abstract
Four cysteine residues (Cys866, Cys917, Cys1094, and Cys1105) have direct roles in cooperatively regulating Janus kinase 2 (JAK2) catalytic activity. Additional site-directed mutagenesis experiments now provide evidence that two of these residues (Cys866 and Cys917) act together as a redox-sensitive switch, allowing JAK2's catalytic activity to be directly regulated by the redox state of the cell. We created several variants of the truncated JAK2 (GST/(NΔ661)rJAK2), which incorporated cysteine-to-serine or cysteine-to-alanine mutations. The catalytic activities of these mutant enzymes were evaluated by in vitro autokinase assays and by in situ autophosphorylation and transphosphorylation assays. Cysteine-to-alanine mutagenesis revealed that the mechanistic role of Cys866 and Cys917 is functionally distinct from that of Cys1094 and Cys1105. Most notable is the observation that the robust activity of the CC866,917AA mutant is unaltered by pretreatment with dithiothreitol or o-iodosobenzoate, unlike all other JAK2 variants previously examined. This work provides the first direct evidence for a cysteine-based redox-sensitive switch that regulates JAK2 catalytic activity. The presence of this redox-sensitive switch predicts that reactive oxygen species can impair the cell's response to JAK-coupled cytokines under conditions of oxidative stress, which we confirm in a murine pancreatic β-islet cell line. | | | 22281400
 |
DNA damage stress and inhibition of Jak2-V617F cause its degradation and synergistically induce apoptosis through activation of GSK3β.
Nagao, T; Oshikawa, G; Wu, N; Kurosu, T; Miura, O
PloS one
6
e27397
2011
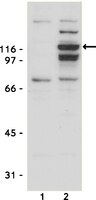
Show Abstract
The cytoplasmic tyrosine kinase Jak2 plays a crucial role in cytokine receptor signaling in hematopoietic cells. The activated Jak2-V617F mutant is present in most cases of BCR/ABL-negative myeloproliferative neoplasms and constitutively activates downstream signals from homodimeric cytokine receptors, such as the erythropoietin receptor (EpoR). Here we examine the effects of DNA damage stress on Jak2 or Jak2-V617F and on induction of apoptosis in hematopoietic cells. Etoposide or doxorubicin dose-dependently decreased the expression level of Jak2 in UT7 or 32D cells expressing EpoR in the absence of Epo and that of exogenously expressed Jak2-V617F in UT7 cells when cotreated with the Jak2 inhibitor JakI-1 or AG490. Studies with pharmacological inhibitors and genetic manipulations further showed that downregulation of the PI3K/Akt pathway leading to the activation of GSK3β may be involved in downregulation of Jak2 or Jak2-V617F as well as in synergistic induction of Bax activation and apoptosis. The downregulation of Jak2 was inhibited by the proteasome inhibitor MG132 or by expression of both of loss-of-function mutants of c-Cbl and Cbl-b, E3 ubiquitin ligases which facilitated ubiquitination of Jak2-V617F when co-expressed in 293T cells. The pan-caspase inhibitor Boc-d-fmk also inhibited the Jak2 downregulation as well as appearance of a 100-kDa fragment that contained the N-terminal portion of Jak2 in response to DNA damage. Together, these data suggest that DNA damage stress with simultaneous inhibition of the kinase activity causes degradation of Jak2 or Jak2-V617F by caspase cleavage and proteasomal degradation through GSK3β activation, which is closely involved in synergistic induction of apoptosis in hematopoietic cells. | | | 22087308
 |
Bone marrow stroma-secreted cytokines protect JAK2(V617F)-mutated cells from the effects of a JAK2 inhibitor.
Manshouri, T; Estrov, Z; Quintás-Cardama, A; Burger, J; Zhang, Y; Livun, A; Knez, L; Harris, D; Creighton, CJ; Kantarjian, HM; Verstovsek, S
Cancer research
71
3831-40
2011
Show Abstract
Signals emanating from the bone marrow microenvironment, such as stromal cells, are thought to support the survival and proliferation of the malignant cells in patients with myeloproliferative neoplasms (MPN). To examine this hypothesis, we established a coculture platform [cells cocultured directly (cell-on-cell) or indirectly (separated by micropore membrane)] designed to interrogate the interplay between Janus activated kinase 2-V617F (JAK2(V617F))-positive cells and the stromal cells. Treatment with atiprimod, a potent JAK2 inhibitor, caused marked growth inhibition and apoptosis of human (SET-2) and mouse (FDCP-EpoR) JAK2(V617F)-positive cells as well as primary blood or bone marrow mononuclear cells from patients with polycythemia vera; however, these effects were attenuated when any of these cell types were cocultured (cell-on-cell) with human marrow stromal cell lines (e.g., HS5, NK.tert, TM-R1). Coculture with stromal cells hampered the ability of atiprimod to inhibit phosphorylation of JAK2 and the downstream STAT3 and STAT5 pathways. This protective effect was maintained in noncontact coculture assays (JAK2(V617F)-positive cells separated by 0.4-μm-thick micropore membranes from stromal cells), indicating a paracrine effect. Cytokine profiling of supernatants from noncontact coculture assays detected distinctly high levels of interleukin 6 (IL-6), fibroblast growth factor (FGF), and chemokine C-X-C-motif ligand 10 (CXCL-10)/IFN-γ-inducible 10-kD protein (IP-10). Anti-IL-6, -FGF, or -CXCL-10/IP-10 neutralizing antibodies ablated the protective effect of stromal cells and restored atiprimod-induced apoptosis of JAK2(V617F)-positive cells. Therefore, our results indicate that humoral factors secreted by stromal cells protect MPN clones from JAK2 inhibitor therapy, thus underscoring the importance of targeting the marrow niche in MPN for therapeutic purposes. | | | 21512135
 |
15-Lipoxygenase-1-enhanced Src-Janus kinase 2-signal transducer and activator of transcription 3 stimulation and monocyte chemoattractant protein-1 expression require redox-sensitive activation of epidermal growth factor receptor in vascular wall remodeling.
Singh, NK; Wang, D; Kundumani-Sridharan, V; Van Quyen, D; Niu, J; Rao, GN
The Journal of biological chemistry
286
22478-88
2011
Show Abstract
To understand the mechanisms by which 15(S)-hydroxyeicosatetraenoic acid (15(S)-HETE) activates signal transducer and activator of transcription 3 (STAT3), we studied the role of epidermal growth factor receptor (EGFR). 15(S)-HETE stimulated tyrosine phosphorylation of EGFR in a time-dependent manner in vascular smooth muscle cells (VSMCs). Interference with EGFR activation blocked 15(S)-HETE-induced Src and STAT3 tyrosine phosphorylation, monocyte chemoattractant protein-1 (MCP-1) expression and VSMC migration. 15(S)-HETE also induced tyrosine phosphorylation of Janus kinase 2 (Jak2) in VSMCs, and its inhibition substantially reduced STAT3 phosphorylation, MCP-1 expression, and VSMC migration. In addition, Src formed a complex with EGFR and Jak2, and its inhibition completely blocked Jak2 and STAT3 phosphorylation, MCP-1 expression, and VSMC migration. 15(S)-HETE induced the production of H(2)O(2) via an NADPH oxidase-dependent manner and its scavengers, N-acetyl cysteine (NAC) and catalase suppressed 15(S)-HETE-stimulated EGFR, Src, Jak2, and STAT3 phosphorylation and MCP-1 expression. Balloon injury (BI) induced EGFR, Src, Jak2, and STAT3 phosphorylation, and inhibition of these signaling molecules attenuated BI-induced MCP-1 expression and smooth muscle cell migration from the medial to the luminal surface resulting in reduced neointima formation. In addition, inhibition of EGFR blocked BI-induced Src, Jak2, and STAT3 phosphorylation. Similarly, interference with Src activation suppressed BI-induced Jak2 and STAT3 phosphorylation. Furthermore, adenovirus-mediated expression of dnJak2 also blocked BI-induced STAT3 phosphorylation. Consistent with the effects of 15(S)-HETE on the activation of EGFR-Src-Jak2-STAT3 signaling in VSMCs in vitro, adenovirus-mediated expression of 15-lipoxygenase 1 (15-Lox1) enhanced BI-induced EGFR, Src, Jak2, and STAT3 phosphorylation leading to enhanced MCP-1 expression in vivo. Blockade of Src or Jak2 suppressed BI-induced 15-Lox1-enhanced STAT3 phosphorylation, MCP-1 expression, and neointima formation. In addition, whereas dominant negative Src blocked BI-induced 15-Lox1-enhanced Jak2 phosphorylation, dnJak2 had no effect on Src phosphorylation. Together, these observations demonstrate for the first time that the 15-Lox1-15(S)-HETE axis activates EGFR via redox-sensitive manner, which in turn mediates Src-Jak2-STAT3-dependent MCP-1 expression leading to vascular wall remodeling. | | | 21536676
 |
A Non-ATP-Competitive Dual Inhibitor of JAK2 and BCR-ABL Kinases: Elucidation of a Novel Therapeutic Spectrum Based on Substrate Competitive Inhibition.
Jatiani, SS; Cosenza, SC; Reddy, MV; Ha, JH; Baker, SJ; Samanta, AK; Olnes, MJ; Pfannes, L; Sloand, EM; Arlinghaus, RB; Reddy, EP
Genes & cancer
1
331-45
2010
Show Abstract
Here we report the discovery of ON044580, an α-benzoyl styryl benzyl sulfide that possesses potent inhibitory activity against two unrelated kinases, JAK2 and BCR-ABL, and exhibits cytotoxicity to human tumor cells derived from chronic myelogenous leukemia (CML) and myelodysplasia (MDS) patients or cells harboring a mutant JAK2 kinase. This novel spectrum of activity is explained by the non-ATP-competitive inhibition of JAK2 and BCR-ABL kinases. ON044580 inhibits mutant JAK2 kinase and the proliferation of JAK2(V617F)-positive leukemic cells and blocks the IL-3-mediated phosphorylation of JAK2 and STAT5. Interestingly, this compound also directly inhibits the kinase activity of both wild-type and imatinib-resistant (T315I) forms of the BCR-ABL kinase. Finally, ON044580 effectively induces apoptosis of imatinib-resistant CML patient cells. The apparently unrelated JAK2 and BCR-ABL kinases share a common substrate, STAT5, and such substrate competitive inhibitors represent an alternative therapeutic strategy for development of new inhibitors. The novel mechanism of kinase inhibition exhibited by ON044580 renders it effective against mutant forms of kinases such as the BCR-ABL(T315I) and JAK2(V617F). Importantly, ON044580 selectively reduces the number of aneuploid cells in primary bone marrow samples from monosomy 7 MDS patients, suggesting another regulatory cascade amenable to this agent in these aberrant cells. Data presented suggest that this compound could have multiple therapeutic applications including monosomy 7 MDS, imatinib-resistant CML, and myeloproliferative neoplasms that develop resistance to ATP-competitive agents. | Western Blotting | | 20717479
 |
Prolactin in ovarian follicular fluid stimulates endothelial cell proliferation.
Alejandra Castilla,Celina García,Martha Cruz-Soto,Gonzalo Martínez de la Escalera,Stéphanie Thebault,Carmen Clapp
Journal of vascular research
47
2010
Show Abstract
Angiogenesis is essential for the growth and maturation of the ovarian follicle and its transition into the corpus luteum. In addition to the main proangiogenic factors, vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF), follicular fluid (FF) contains the hormone prolactin (PRL), which is known to promote angiogenesis in vivo. Here, we show that FF from large follicles, which contains twice the PRL level of FF from small follicles, stimulates endothelial cell proliferation to a greater extent than the latter, and that immunoneutralization of PRL prevents FF from stimulating endothelial cell proliferation. Notably, the FF increases the expression of the short and long PRL receptor isoforms in endothelial cells, and a purified PRL standard stimulates endothelial cell proliferation but only after the cells have been pretreated with FF. However, purified PRL activates the JAK2/STAT3 pathway in endothelial cells in the absence of pretreatment with FF. In summary, PRL present in the FF stimulates the proliferation of endothelial cells. This effect likely involves the upregulation of the short and long PRL receptor isoforms and is independent of PRL-induced JAK2/STAT3 signaling. | | | 19672107
 |

















[04-1098_IH(P)-ALL].jpg)