Human Embryonic Stem Cell-Derived Progenitors Assist Functional Sensory Axon Regeneration after Dorsal Root Avulsion Injury.
Hoeber, J; Trolle, C; Konig, N; Du, Z; Gallo, A; Hermans, E; Aldskogius, H; Shortland, P; Zhang, SC; Deumens, R; Kozlova, EN
Scientific reports
5
10666
2015
Show Abstract
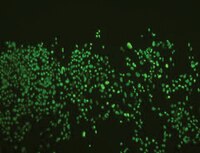
Dorsal root avulsion results in permanent impairment of sensory functions due to disconnection between the peripheral and central nervous system. Improved strategies are therefore needed to reconnect injured sensory neurons with their spinal cord targets in order to achieve functional repair after brachial and lumbosacral plexus avulsion injuries. Here, we show that sensory functions can be restored in the adult mouse if avulsed sensory fibers are bridged with the spinal cord by human neural progenitor (hNP) transplants. Responses to peripheral mechanical sensory stimulation were significantly improved in transplanted animals. Transganglionic tracing showed host sensory axons only in the spinal cord dorsal horn of treated animals. Immunohistochemical analysis confirmed that sensory fibers had grown through the bridge and showed robust survival and differentiation of the transplants. Section of the repaired dorsal roots distal to the transplant completely abolished the behavioral improvement. This demonstrates that hNP transplants promote recovery of sensorimotor functions after dorsal root avulsion, and that these effects are mediated by spinal ingrowth of host sensory axons. These results provide a rationale for the development of novel stem cell-based strategies for functionally useful bridging of the peripheral and central nervous system. | Immunohistochemistry | | 26053681
 |
Development and rescue of human familial hypercholesterolaemia in a xenograft mouse model.
Bissig-Choisat, B; Wang, L; Legras, X; Saha, PK; Chen, L; Bell, P; Pankowicz, FP; Hill, MC; Barzi, M; Leyton, CK; Leung, HC; Kruse, RL; Himes, RW; Goss, JA; Wilson, JM; Chan, L; Lagor, WR; Bissig, KD
Nature communications
6
7339
2015
Show Abstract
Diseases of lipid metabolism are a major cause of human morbidity, but no animal model entirely recapitulates human lipoprotein metabolism. Here we develop a xenograft mouse model using hepatocytes from a patient with familial hypercholesterolaemia caused by loss-of-function mutations in the low-density lipoprotein receptor (LDLR). Like familial hypercholesterolaemia patients, our familial hypercholesterolaemia liver chimeric mice develop hypercholesterolaemia and a 'humanized' serum profile, including expression of the emerging drug targets cholesteryl ester transfer protein and apolipoprotein (a), for which no genes exist in mice. We go on to replace the missing LDLR in familial hypercholesterolaemia liver chimeric mice using an adeno-associated virus 9-based gene therapy and restore normal lipoprotein profiles after administration of a single dose. Our study marks the first time a human metabolic disease is induced in an experimental animal model by human hepatocyte transplantation and treated by gene therapy. Such xenograft platforms offer the ability to validate human experimental therapies and may foster their rapid translation into the clinic. | | | 26081744
 |
Enhancement of Ischemic Wound Healing by Spheroid Grafting of Human Adipose-Derived Stem Cells Treated with Low-Level Light Irradiation.
Park, IS; Chung, PS; Ahn, JC
PloS one
10
e0122776
2015
Show Abstract
We investigated whether low-level light irradiation prior to transplantation of adipose-derived stromal cell (ASC) spheroids in an animal skin wound model stimulated angiogenesis and tissue regeneration to improve functional recovery of skin tissue. The spheroid, composed of hASCs, was irradiated with low-level light and expressed angiogenic factors, including vascular endothelial growth factor (VEGF), basic fibroblast growth factor (FGF), and hepatocyte growth factor (HGF). Immunochemical staining analysis revealed that the spheroid of the hASCs was CD31+, KDR+, and CD34+. On the other hand, monolayer-cultured hASCs were negative for these markers. PBS, human adipose tissue-derived stromal cells, and the ASC spheroid were transplanted into a wound bed in athymic mice to evaluate the therapeutic effects of the ASC spheroid in vivo. The ASC spheroid transplanted into the wound bed differentiated into endothelial cells and remained differentiated. The density of vascular formations increased as a result of the angiogenic factors released by the wound bed and enhanced tissue regeneration at the lesion site. These results indicate that the transplantation of the ASC spheroid significantly improved functional recovery relative to both ASC transplantation and PBS treatment. These findings suggest that transplantation of an ASC spheroid treated with low-level light may be an effective form of stem cell therapy for treatment of a wound bed. | | | 26065900
 |
The Anti-Tumor Effects of Adipose Tissue Mesenchymal Stem Cell Transduced with HSV-Tk Gene on U-87-Driven Brain Tumor.
de Melo, SM; Bittencourt, S; Ferrazoli, EG; da Silva, CS; da Cunha, FF; da Silva, FH; Stilhano, RS; Denapoli, PM; Zanetti, BF; Martin, PK; Silva, LM; dos Santos, AA; Baptista, LS; Longo, BM; Han, SW
PloS one
10
e0128922
2015
Show Abstract
Glioblastoma (GBM) is an infiltrative tumor that is difficult to eradicate. Treating GBM with mesenchymal stem cells (MSCs) that have been modified with the HSV-Tk suicide gene has brought significant advances mainly because MSCs are chemoattracted to GBM and kill tumor cells via a bystander effect. To use this strategy, abundantly present adipose-tissue-derived mesenchymal stem cells (AT-MSCs) were evaluated for the treatment of GBM in mice. AT-MSCs were prepared using a mechanical protocol to avoid contamination with animal protein and transduced with HSV-Tk via a lentiviral vector. The U-87 glioblastoma cells cultured with AT-MSC-HSV-Tk died in the presence of 25 or 50 μM ganciclovir (GCV). U-87 glioblastoma cells injected into the brains of nude mice generated tumors larger than 3.5 mm2 after 4 weeks, but the injection of AT-MSC-HSV-Tk cells one week after the U-87 injection, combined with GCV treatment, drastically reduced tumors to smaller than 0.5 mm2. Immunohistochemical analysis of the tumors showed the presence of AT-MSC-HSV-Tk cells only within the tumor and its vicinity, but not in other areas of the brain, showing chemoattraction between them. The abundance of AT-MSCs and the easier to obtain them mechanically are strong advantages when compared to using MSCs from other tissues. | | | 26067671
 |
A Subsequent Human Neural Progenitor Transplant into the Degenerate Retina Does Not Compromise Initial Graft Survival or Therapeutic Efficacy.
Lu, B; Lin, Y; Tsai, Y; Girman, S; Adamus, G; Jones, MK; Shelley, B; Svendsen, CN; Wang, S
Translational vision science & technology
4
7
2015
Show Abstract
Stem and progenitor cell transplantation provides a promising clinical application for treating degenerative retinal diseases, including age-related macular degeneration (AMD) and retinitis pigmentosa (RP). Our previous studies have shown that a single subretinal injection of human cortical-derived neural progenitor cells (hNPC(ctx)) into cyclosporine-treated Royal College of Surgeons (RCS) rats preserved both photoreceptors and visual function. However, it is still unknown whether nonautologous progenitor cell readministration for sustained vision is efficacious and safe in terms of the initial graft initiating an immune response to a subsequent graft.A cell suspension containing 3×10(4) hNPC(ctx) into one eye of cyclosporine-treated RCS rats at postnatal day 21 (P21), followed by a second transplantation at P95 into the previously untreated fellow eye.hNPC(ctx) delayed photoreceptor degeneration and preserved visual function, as measured by electroretinography (ERG), optokinetic response (OKR), and luminance threshold recordings (LTRs). Visual function and photoreceptors of the initially treated eye were still preserved 6 weeks after hNPC(ctx) were injected into the second eye. Antibodies against T-cell markers showed that CD3, CD4, and CD8 T cells were not detected at P90 and P140 in most cases. No detectable level of anti-nestin antibody was found in serum by enzyme-linked immunosorbent assay (ELISA).This xenograft study with cyclosporine-treated animals demonstrates that readministration of hNPC(ctx) into the fellow eye did not induce anti-graft immune responses or lower therapeutic efficacy of hNPC(ctx) in preserving vision. Thus, readministration of progenitor cells to sustain long-term efficacy may be an option for long-term therapies of retinal degeneration.Redosing neural progenitors do not affect the efficacy of the initial grafts in protecting vision or induce unwanted immune responses. | | | 25694843
 |
Umbilical cord mesenchymal stem cells modulate dextran sulfate sodium induced acute colitis in immunodeficient mice.
Banerjee, A; Bizzaro, D; Burra, P; Di Liddo, R; Pathak, S; Arcidiacono, D; Cappon, A; Bo, P; Conconi, MT; Crescenzi, M; Pinna, CM; Parnigotto, PP; Alison, MR; Sturniolo, GC; D'Incà, R; Russo, FP
Stem cell research & therapy
6
79
2015
Show Abstract
Inflammatory bowel diseases (IBD) are complex multi-factorial diseases with increasing incidence worldwide but their treatment is far from satisfactory. Unconventional strategies have consequently been investigated, proposing the use of cells as an effective alternative approach to IBD. In the present study we examined the protective potential of exogenously administered human umbilical cord derived mesenchymal stem cells (UCMSCs) against Dextran Sulfate Sodium (DSS) induced acute colitis in immunodeficient NOD.CB17-Prkdc (scid)/J mice with particular attention to endoplasmic reticulum (ER) stress.UCMSCs were injected in NOD.CB17-Prkdc (scid)/J via the tail vein at day 1 and 4 after DSS administration. To verify attenuation of DSS induced damage by UCMSCs, Disease Activity Index (DAI) and body weight changes was monitored daily. Moreover, colon length, histological changes, myeloperoxidase and catalase activities, metalloproteinase (MMP) 2 and 9 expression and endoplasmic reticulum (ER) stress related proteins were evaluated on day 7.UCMSCs administration to immunodeficient NOD.CB17-Prkdc (scid)/J mice after DSS damage significantly reduced DAI (1.45 ± 0.16 vs 2.08 ± 0.18, p less than 0.05), attenuating the presence of bloody stools, weight loss, colon shortening (8.95 ± 0.33 cm vs 6.8 ± 0.20 cm, p less than 0.01) and histological score (1.97 ± 0.13 vs 3.27 ± 0.13, p less than 0.001). Decrease in neutrophil infiltration was evident from lower MPO levels (78.2 ± 9.7 vs 168.9 ± 18.2 U/g, p less than 0.01). DSS treatment enhanced MMP2 and MMP9 activities (greater than 3-fold), which were significantly reduced in mice receiving UCMSCs. Moreover, positive modulation in ER stress related proteins was observed after UCMSCs administration.Our results demonstrated that UCMSCs are able to prevent DSS-induced colitis in immunodeficient mice. Using these mice we demonstrated that our UCMSCs have a direct preventive effect other than the T-cell immunomodulatory properties which are already known. Moreover we demonstrated a key function of MMPs and ER stress in the establishment of colitis suggesting them to be potential therapeutic targets in IBD treatment. | | | 25890182
 |
Early detection of structural abnormalities and cytoplasmic accumulation of TDP-43 in tissue-engineered skins derived from ALS patients.
Paré, B; Touzel-Deschênes, L; Lamontagne, R; Lamarre, MS; Scott, FD; Khuong, HT; Dion, PA; Bouchard, JP; Gould, P; Rouleau, GA; Dupré, N; Berthod, F; Gros-Louis, F
Acta neuropathologica communications
3
5
2015
Show Abstract
Amyotrophic lateral sclerosis (ALS) is an adult-onset disease characterized by the selective degeneration of motor neurons in the brain and spinal cord progressively leading to paralysis and death. Current diagnosis of ALS is based on clinical assessment of related symptoms. The clinical manifestations observed in ALS appear relatively late in the disease course after degeneration of a significant number of motor neurons. As a result, the identification and development of disease-modifying therapies is difficult. Therefore, novel strategies for early diagnosis of neurodegeneration, to monitor disease progression and to assess response to existing and future treatments are urgently needed. Factually, many neurological disorders, including ALS, are accompanied by skin changes that often precede the onset of neurological symptoms. Aiming to generate an innovative human-based model to facilitate the identification of predictive biomarkers associated with the disease, we developed a unique ALS tissue-engineered skin model (ALS-TES) derived from patient's own cells. The ALS-TES presents a number of striking features including altered epidermal differentiation, abnormal dermo-epidermal junction, delamination, keratinocyte infiltration, collagen disorganization and cytoplasmic TDP-43 inclusions. Remarkably, these abnormal skin defects, uniquely seen in the ALS-derived skins, were detected in pre-symtomatic C9orf72-linked ALS patients carrying the GGGGCC DNA repeat expansion. Consequently, our ALS skin model could represent a renewable source of human tissue, quickly and easily accessible to better understand the physiophatological mechanisms underlying this disease, to facilitate the identification of disease-specific biomarkers, and to develop innovative tools for early diagnosis and disease monitoring. | | | 25637145
 |
Intravenous Bone Marrow Stem Cell Grafts Preferentially Migrate to Spleen and Abrogate Chronic Inflammation in Stroke.
Acosta, SA; Tajiri, N; Hoover, J; Kaneko, Y; Borlongan, CV
Stroke; a journal of cerebral circulation
46
2616-27
2015
Show Abstract
Adult stem cell therapy is an experimental stroke treatment. Here, we assessed homing and anti-inflammatory effects of bone marrow stromal cells (hBMSCs) in chronic stroke.At 60 days post stroke, adult Sprague-Dawley rats received intravenous hBMSCs (4×10(6) labeled or nonlabeled cells) or vehicle (saline). A sham surgery group served as additional control. In vivo imaging was conducted between 1 hour and 11 days post transplantation, followed by histological examination.Labeled hBMSCs migrated to spleen which emitted significantly higher fluorescent signal across all time points, especially during the first hour, and were modestly detected in the head region at the 12 hours and 11 days, compared with nonlabeled hBMSCs and vehicle-infused stroke animals, or sham (Pless than 0.05). At 11 days post transplantation, ex vivo imaging confirmed preferential hBMSC migration to the spleen over the brain. Hematoxylin and eosin staining revealed significant 15% and 30% reductions in striatal infarct and peri-infarct area, and a trend of rescue against neuronal loss in the hippocampus. Unbiased stereology showed significant 75% and 60% decrements in major histocompatibility complex II-activated inflammatory cells in gray and white matter, and a 43% diminution in tumor necrosis factor-α cell density in the spleen of transplanted stroke animals compared with vehicle-infused stroke animals (Pless than 0.05). Human antigen immunostaining revealed 0.03% hBMSCs survived in spleen and only 0.0007% in brain. MSC migration to spleen, but not brain, inversely correlated with reduced infarct, peri-infarct, and inflammation.hBMSC transplantation is therapeutic in chronic stroke possibly by abrogating the inflammation-plagued secondary cell death. | | | 26219646
 |
Non-Invasive In Vivo Imaging and Quantification of Tumor Growth and Metastasis in Rats Using Cells Expressing Far-Red Fluorescence Protein.
Christensen, J; Vonwil, D; Shastri, VP
PloS one
10
e0132725
2015
Show Abstract
Non-invasive in vivo imaging is emerging as an important tool for basic and preclinical research. Near-infrared (NIR) fluorescence dyes and probes have been used for non-invasive optical imaging since in the NIR region absorption and auto fluorescence by body tissue is low, thus permitting for greater penetration depths and high signal to noise ratio. Currently, cell tracking systems rely on labeling cells prior to injection or administering probes targeting the cell population of choice right before imaging. These approaches do not enable imaging of tumor growth, as the cell label is diluted during cell division. In this study we have developed cell lines stably expressing the far-red fluorescence protein E2-Crimson, thus enabling continuous detection and quantification of tumor growth. In a xenograft rat model, we show that E2-Crimson expressing cells can be detected over a 5 week period using optical imaging. Fluorescence intensities correlated with tumor volume and weight and allowed for a reliable and robust quantification of the entire tumor compartment. Using a novel injection regime, the seeding of MDA-MB-231 breast cancer cells in the lungs in a rat model was established and verified. | | | 26186005
 |
Transplantation of human Wharton's jelly-derived mesenchymal stem cells highly expressing TGFβ receptors in a rabbit model of disc degeneration.
Ahn, J; Park, EM; Kim, BJ; Kim, JS; Choi, B; Lee, SH; Han, I
Stem cell research & therapy
6
190
2015
Show Abstract
Mesenchymal stem cells (MSCs) are widely considered to hold promise for the treatment of intervertebral disc (IVD) degeneration. However, variation in the therapeutic efficacy of MSCs is a major problem and the derivation of MSCs for use in IVD regeneration has not been optimized. Additionally, no data are available on the efficacy of Wharton's Jelly-derived MSC (WJ-MSC) transplantation in an animal model of IVD degeneration.This study evaluated the effectiveness of a cross-linked hyaluronic acid (XHA) scaffold loaded with human WJ-MSCs, according to their expression levels of transforming growth factor-β receptor I/activin-like kinase receptor 5 (TβRI/ALK5) and TβRII, for IVD regeneration in a rabbit model. We compared the degree of IVD regeneration between rabbits transplanted with a XHA scaffold loaded with WJ-MSCs highly and lowly expressing TβRI/ALK5 and TβRII (MSC-highTR and MSC-lowTR, respectively) using magnetic resonance imaging (MRI) and histological analysis.At 12 weeks after transplantation, T2-weighted MRI analysis showed significant restoration of the disc water content in rabbits treated with a MSC-highTR-loaded XHA scaffold in comparison to rabbits treated with the scaffold alone or a MSC-lowTR-loaded XHA scaffold. In addition, morphological and histological analyses revealed that IVD regeneration was highest in rabbits transplanted with a MSC-highTR-loaded XHA scaffold.Taken together, our results suggest that a MSC-highTR-loaded XHA scaffold supports IVD regeneration more effectively than a MSC-lowTR-loaded XHA scaffold. This study supports the potential clinical use of MSC-highTR-loaded XHA scaffolds to halt IVD degeneration or to enhance IVD regeneration. | | | 26432097
 |